AI to the Rescue: How MIT is Designing a New Generation of Antibiotics to Combat Superbugs
The Silent Pandemic: A World Running Out of Cures
For decades, a silent pandemic has been spreading across the globe, not with the explosive speed of a virus, but with the slow, relentless creep of evolution. This is the crisis of antibiotic resistance. The miracle drugs that defined modern medicine, turning once-deadly infections into treatable conditions, are losing their power. Bacteria, in their constant struggle for survival, have evolved to outsmart our best chemical weapons, giving rise to "superbugs" that are resistant to multiple, and sometimes all, available antibiotics. The World Health Organization has declared this one of the top global public health threats facing humanity, a crisis that could plunge us back into a pre-antibiotic era where a simple cut or a routine surgery could become a life-threatening event.
For years, the pipeline for new antibiotics has been running dry. The traditional methods of drug discovery—screening vast libraries of natural and synthetic compounds—are slow, expensive, and yield diminishing returns. Most new antibiotics approved in recent decades have been mere modifications of existing drug classes, offering only a temporary reprieve as bacteria inevitably develop resistance to them as well. The world has been in desperate need of a new approach, a revolutionary tool to discover truly novel weapons in our war against these microscopic foes. Now, a breakthrough from the Massachusetts Institute of Technology (MIT) suggests that help has arrived, and it comes in the form of artificial intelligence.

A Digital Breakthrough: Generative AI Designs Novel Antibiotics
In a landmark study, a team of researchers at MIT has successfully used generative AI to design entirely new classes of antibiotics that are effective against some of the world's most dangerous drug-resistant bacteria, including the notorious MRSA (methicillin-resistant Staphylococcus aureus) and the bacteria responsible for gonorrhea. This isn't just about using AI to screen existing molecules faster; it's about using AI to create and invent brand-new molecules from scratch, with structures and mechanisms of action unlike any known antibiotic.
This achievement marks a pivotal moment in the fight against antibiotic resistance. It proves that AI can be a powerful creative partner in drug discovery, capable of exploring a vast, uncharted chemical space to find solutions that have eluded human scientists for decades. As Professor James Collins, a leading figure in biomedical engineering at MIT, explains, "We are using AI not just to screen existing molecular libraries, but to generate new molecules in unexplored chemical spaces. This opens up a previously impossible discovery area for antibiotic development."

The Two-Pronged AI Attack: Fragment-Based and Free Design
The MIT team employed a sophisticated, two-pronged strategy to unleash the creative power of their AI models.
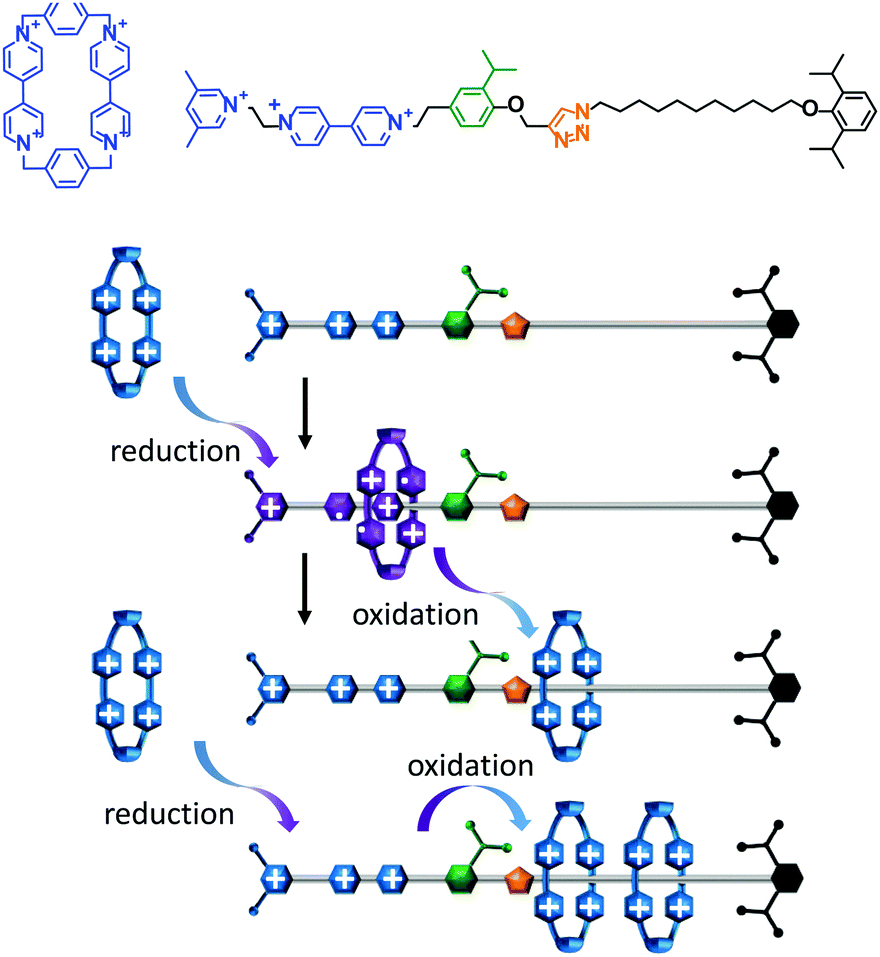
1. Fragment-Based Design: Intelligent Assembly
The first approach, known as "fragment-based design," is akin to giving the AI a set of advanced LEGO bricks. The process began by identifying small chemical fragments or building blocks that were likely to have some antibacterial properties. The AI models sifted through a colossal library of 45 million such fragments, filtering out any that were toxic to humans or too similar to existing antibiotics. This narrowed the field to about one million promising candidates.
From this pool, a selected fragment was fed to generative AI algorithms (specifically, models named CReM and F-VAE). These algorithms then went to work, intelligently combining and modifying the fragment to generate millions of new, complete molecular structures. One of the most promising molecules to emerge from this process was named NG1. In both laboratory tests and subsequent trials in animal models, NG1 proved to be remarkably effective at eradicating drug-resistant strains of Neisseria gonorrhoeae, the bacterium that causes gonorrhea.
2. Free Design: Unconstrained Creativity
The second approach was even more ambitious. In this "free design" method, the AI was given complete creative freedom, with no starting fragments to constrain it. Using the same powerful CReM and VAE algorithms, the AI generated over 29 million entirely theoretical molecules from the ground up.
After a rigorous filtering process to select for synthesizability and predicted efficacy, 90 candidates were chosen for further study. Of these, 22 were successfully synthesized, and an incredible six of them showed potent antibacterial activity against MRSA, the infamous "hospital superbug." The standout from this group, a molecule dubbed DN1, was so effective that it successfully treated MRSA skin infections in mouse models.

A New Arsenal: Novel Structures, Novel Mechanisms
What makes the discovery of NG1 and DN1 so revolutionary is that they are structurally unlike any known antibiotic. This is not just another variation on a penicillin or a tetracycline. This is something entirely new, which means bacteria have not had the evolutionary opportunity to develop resistance to them.
Even more exciting is how they work. The researchers found that NG1 targets a specific protein called LptA, which is crucial for building the outer membrane of the gonorrhea bacterium. By disrupting this process, NG1 effectively causes the bacterium's protective wall to crumble, leading to cell death. DN1, on the other hand, appears to work through broader mechanisms that disrupt the integrity of the bacterial membrane.
This ability to discover drugs with entirely new mechanisms of action is the holy grail of antibiotic research. It offers a way to bypass the resistance mechanisms that bacteria have developed against existing drugs and provides a much-needed infusion of innovation into the field. It demonstrates that AI can move beyond simply identifying derivatives of known drugs and can instead become a true engine for fundamental discovery.
The Dawn of AI-Driven Drug Discovery
The implications of this research extend far beyond the two molecules discovered. It provides a blueprint for a new era of drug discovery, one that is faster, more efficient, and vastly more creative. The ability of AI to design, test, and validate new drug candidates in a virtual space before any costly and time-consuming laboratory work is done can dramatically accelerate the pace of medical innovation.
The MIT team is already looking ahead. Their immediate goal is to optimize NG1 and DN1 for preclinical testing, the next critical step on the long road to clinical use in humans. But their ambition doesn't stop there. They plan to turn their powerful AI platform against other deadly pathogens, including Mycobacterium tuberculosis (the cause of tuberculosis) and Pseudomonas aeruginosa, another notoriously difficult-to-treat bacterium.
A New Hope in the War Against Superbugs
For decades, the story of antibiotic resistance has been one of growing despair, a narrative of a race we seemed destined to lose. The MIT breakthrough offers a powerful new narrative of hope and ingenuity. It shows that by combining the creative power of artificial intelligence with the deep expertise of human scientists, we can open up new frontiers in the fight against infectious diseases.
While NG1 and DN1 are still years away from appearing in our medicine cabinets, their discovery is a monumental proof of concept. It signals that we now have a powerful new ally in our corner. The age of AI-driven drug discovery has dawned, and with it comes the promise of a future where humanity can once again gain the upper hand in our ancient war against bacteria. The silent pandemic has a new, formidable adversary.
The Science Behind the Breakthrough: Understanding Generative AI in Drug Discovery
To truly appreciate the magnitude of this achievement, it's essential to understand the sophisticated science behind it. Generative AI, the technology that has captured the world's attention through applications like ChatGPT and DALL-E, works by learning patterns from vast datasets and then using those patterns to create new content. In the case of drug discovery, the AI models were trained on enormous databases of molecular structures and their biological activities.
The key innovation lies in the AI's ability to understand the relationship between a molecule's structure and its function. Traditional drug discovery relies heavily on human intuition and experience to predict which molecular modifications might improve a drug's effectiveness or reduce its side effects. This process is slow, expensive, and often unsuccessful. AI, however, can process and analyze molecular relationships at a scale and speed that is simply impossible for human researchers.
The CReM (Chemical Reaction and Molecular) algorithm used by the MIT team is particularly sophisticated. It doesn't just randomly combine molecular fragments; it understands the rules of chemistry and can predict which combinations are likely to be stable and synthesizable. The F-VAE (Fragment Variational Autoencoder) adds another layer of intelligence by learning to represent molecular fragments in a mathematical space where similar fragments are close together, allowing the AI to make intelligent substitutions and modifications.
This combination of algorithms creates a powerful engine for molecular creativity. The AI can explore millions of potential molecular structures in a matter of hours, something that would take human chemists decades to accomplish. More importantly, it can venture into areas of chemical space that human researchers might never think to explore, uncovering entirely new classes of compounds with unexpected properties.

The Global Context: A Race Against Time
The urgency of developing new antibiotics cannot be overstated. According to the Centers for Disease Control and Prevention, antibiotic-resistant infections cause more than 2.8 million infections and 35,000 deaths each year in the United States alone. Globally, the numbers are even more staggering, with some estimates suggesting that antibiotic resistance could cause 10 million deaths annually by 2050 if left unchecked.
The economic impact is equally devastating. The World Bank estimates that antibiotic resistance could reduce global GDP by 1.1% to 3.8% by 2050, with the poorest countries bearing the heaviest burden. Healthcare costs are skyrocketing as doctors are forced to use more expensive, last-resort antibiotics, and patients require longer hospital stays for infections that were once easily treatable.
Perhaps most concerning is the impact on modern medicine itself. Many of the medical procedures we take for granted—from routine surgeries to cancer chemotherapy—depend on our ability to prevent and treat infections. As antibiotics lose their effectiveness, these procedures become increasingly risky, potentially forcing us to abandon some of the greatest achievements of modern medicine.
The MIT breakthrough comes at a critical juncture in this crisis. While pharmaceutical companies have largely abandoned antibiotic research due to poor financial returns, academic institutions and government agencies are stepping up to fill the gap. The use of AI in drug discovery offers a way to dramatically reduce the cost and time required to develop new antibiotics, potentially making antibiotic research economically viable once again.

Beyond Antibiotics: The Broader Implications for Medicine
While the immediate focus of the MIT research is on antibiotics, the implications extend far beyond infectious diseases. The same AI techniques that were used to design NG1 and DN1 could be applied to virtually any area of drug discovery. Cancer treatments, neurological disorders, autoimmune diseases—all could benefit from this approach.
The pharmaceutical industry is already taking notice. Major drug companies are investing heavily in AI-driven drug discovery platforms, recognizing that this technology could revolutionize how new medicines are developed. The traditional model of drug discovery, which can take 10-15 years and cost billions of dollars, is ripe for disruption.
AI offers the promise of a more efficient, targeted approach to drug development. Instead of screening thousands of compounds in the hope of finding one that works, AI can design molecules specifically tailored to target particular diseases or biological pathways. This precision approach could lead to more effective treatments with fewer side effects, bringing us closer to the goal of personalized medicine.
The MIT research also demonstrates the power of interdisciplinary collaboration. The breakthrough was made possible by bringing together experts in artificial intelligence, chemistry, biology, and medicine. This kind of cross-pollination of ideas is essential for tackling complex challenges like antibiotic resistance and will likely become increasingly important as science becomes more specialized and interconnected.
Challenges and Limitations: The Road Ahead
Despite the excitement surrounding this breakthrough, it's important to acknowledge the challenges that lie ahead. NG1 and DN1 are still in the early stages of development, and there's no guarantee that they will ultimately prove safe and effective in humans. The journey from laboratory discovery to approved drug is long and fraught with obstacles.
One of the biggest challenges is ensuring that these new antibiotics are truly safe for human use. While the AI models were trained to avoid molecules that are likely to be toxic, predicting toxicity is notoriously difficult, and unexpected side effects can emerge during clinical trials. The researchers will need to conduct extensive safety testing before these compounds can be tested in humans.
Another challenge is the question of resistance. While NG1 and DN1 work through novel mechanisms that bacteria haven't encountered before, evolution is relentless. Given enough time and exposure, bacteria will likely develop resistance to these new drugs as well. This means that even as we celebrate these discoveries, we must continue to develop new antibiotics to stay ahead of bacterial evolution.
The regulatory pathway for new antibiotics is also complex and expensive. Getting a new antibiotic approved by regulatory agencies like the FDA requires extensive clinical trials that can cost hundreds of millions of dollars. For academic institutions like MIT, finding the resources to fund these trials can be a significant challenge.
There are also broader questions about how AI-designed drugs should be regulated. Current regulatory frameworks were designed for traditionally discovered drugs, and it's not clear how they should be adapted for AI-generated compounds. Regulators will need to develop new guidelines for evaluating the safety and efficacy of AI-designed drugs, a process that could take years.

The Future of AI in Medicine: A Paradigm Shift
Looking beyond the immediate challenges, the MIT breakthrough represents a fundamental shift in how we approach medical research. For the first time in history, we have machines that can truly participate in the creative process of drug discovery, not just as tools for analysis but as partners in innovation.
This partnership between human intelligence and artificial intelligence is likely to become the dominant model for medical research in the coming decades. Humans bring intuition, creativity, and deep biological understanding, while AI contributes computational power, pattern recognition, and the ability to explore vast solution spaces. Together, they form a formidable team capable of tackling challenges that neither could address alone.
The implications extend beyond drug discovery to virtually every aspect of medicine. AI is already being used to analyze medical images, predict disease outcomes, and personalize treatment plans. As these technologies mature, we can expect to see AI playing an increasingly central role in healthcare, from diagnosis and treatment to prevention and public health.
The MIT research also highlights the importance of open science and collaboration in addressing global health challenges. The researchers have made their AI models and findings publicly available, allowing other scientists around the world to build on their work. This open approach accelerates progress and ensures that the benefits of these discoveries can be shared globally, particularly important for addressing challenges like antibiotic resistance that affect all of humanity.

A New Chapter in the Fight Against Disease
The development of NG1 and DN1 marks the beginning of a new chapter in humanity's long struggle against infectious disease. For the first time since the discovery of penicillin nearly a century ago, we have a fundamentally new approach to finding antibiotics—one that promises to be faster, more efficient, and more creative than anything that came before.
This breakthrough comes at a critical moment when the world desperately needs new weapons in the fight against antibiotic resistance. The COVID-19 pandemic has reminded us of our vulnerability to infectious diseases and the importance of having effective treatments available. The MIT research offers hope that we can stay ahead of bacterial evolution and continue to protect human health in an age of increasing antimicrobial resistance.
As we look to the future, it's clear that artificial intelligence will play an increasingly important role in medicine and drug discovery. The success of the MIT team in designing novel antibiotics is just the beginning. With continued investment in AI research and development, we can expect to see even more dramatic breakthroughs in the years to come.
The fight against antibiotic resistance is far from over, but for the first time in decades, we have reason for optimism. The combination of human ingenuity and artificial intelligence has opened up new possibilities for drug discovery that were unimaginable just a few years ago. As we continue to develop and refine these technologies, we move closer to a future where infectious diseases no longer pose an existential threat to human civilization.
The age of AI-driven medicine has begun, and with it comes the promise of better health outcomes for people around the world. The MIT breakthrough is not just a scientific achievement; it's a beacon of hope in our ongoing battle against the microscopic enemies that have plagued humanity throughout history. In this new era, we are no longer fighting alone—we have artificial intelligence as our ally, and together, we are stronger than ever before.